- Welcome to Anil Mandhani
- Call for Appointment +918920721799
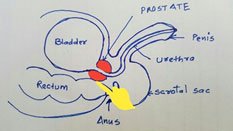
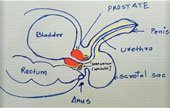
What is Prostate Cancer?
Prostate cancer (PC) is a type of cancer that affects the prostate gland, which is located at the base of the bladder. The prostate plays a role in nourishing sperm by producing a fluid that is part of semen. It also produces Prostate-Specific Antigen (PSA), a protein that helps in liquefying semen for better sperm mobility.

Risk of Developing Prostate Cancer
The lifetime risk of having microscopic prostate cancer for a 50-year-old man is approximately 42%, but the risk of dying from it is around 3%. In North America, about 100 out of 100,000 men develop prostate cancer, whereas in Asia, the number is about 5 per 100,000. While the overall risk is lower in India, due to its large population, many cases are observed, especially in men aged 55 to 70 years.
Symptoms of Prostate Cancer
In its early stages, prostate cancer usually does not cause symptoms. However, in advanced stages, it can lead to urinary obstruction or blood in the urine. Most urinary symptoms in older men are caused by benign prostate enlargement (BPH), not cancer.
Risk Factors for Prostate Cancer
Although the exact cause of prostate cancer remains unknown, certain factors can increase the risk. Some measures that may help reduce the risk include:
- Regular exercise
- Regular sexual activity
- Reducing red meat consumption
- Avoiding smoking and tobacco use
- Maintaining a healthy weight and avoiding obesity
Early Detection and Screening
Since early-stage prostate cancer does not produce symptoms, screening is crucial for early detection. The PSA test is recommended for men aged 55 to 70, or earlier (at age 45) for those with a family history of prostate cancer. In India, PSA testing is done opportunistically, meaning it is usually recommended when men visit a urologist for urinary symptoms or during executive health check-ups.
What is PSA Screening?
The PSA test was introduced in 1986 and has since been widely used in Western countries to detect prostate cancer early. In North America, 95% of prostate cancers are detected at an early stage due to PSA screening. In India, due to the lack of routine screening, more than 50-60% of prostate cancer cases are diagnosed at an advanced stage. However, executive health check-ups and the availability of robotic surgery have led to an increase in early-stage detection.
Tests to Confirm Diagnosis
- Rectal Examination – A urologist performs a digital rectal exam (DRE) by inserting a finger into the rectum to check for any hardness or nodules in the prostate.
- Blood PSA Test – PSA levels in the blood can indicate prostate cancer. However, high PSA levels are not always due to cancer; benign prostatic hyperplasia (BPH), infections, and even recent ejaculation can temporarily increase PSA levels. In India, the PSA threshold for biopsy in symptomatic men is set at 5.4 ng/ml.
- MRI of the Prostate – This imaging test helps assess whether the cancer has spread beyond the prostate and evaluates lymph node involvement. A scoring system called PIRADS (Prostate Imaging Reporting and Data System) helps determine the need for a biopsy. It is preferable to do an MRI before a biopsy or at least 6-8 weeks after a biopsy.
- PSMA PET CT is another useful tool to stage cancer for metastasis. This is a useful adjunct in a situation, where patients present with High PSA and very high Gleason grades.
What is a Prostate Biopsy?
A prostate biopsy involves taking small tissue samples (typically 10-12) from the prostate using a needle inserted through the rectum under local anesthesia. The samples are then analyzed by a pathologist. This procedure may cause temporary discomfort, mild pain, and blood in the urine for a few days. A clean rectum and a short course of antibiotics are recommended before the biopsy.
Stages of Prostate Cancer
Prostate cancer is classified into three main stages:
- Localized Prostate Cancer – Confined to the prostate gland and can be treated with curative intent.
- Locally Advanced Prostate Cancer – Has started to spread beyond the prostate and may require additional therapies such as hormonal or radiation therapy along with surgery.
- Metastatic Prostate Cancer – Cancer has spread to other parts of the body. Though not curable, it can be managed with hormonal therapy and chemotherapy to prolong life.
Treatment Options
- Localized Prostate Cancer (Group 1): Radical prostatectomy (robotic, laparoscopic, or open surgery) or radical radiotherapy. Surgery is preferred if the patient has urinary obstruction.
- Locally Advanced Prostate Cancer (Group 2): Surgery or radiation therapy combined with hormonal treatment.
- Metastatic Prostate Cancer (Group 3): Hormonal therapy and/or chemotherapy.
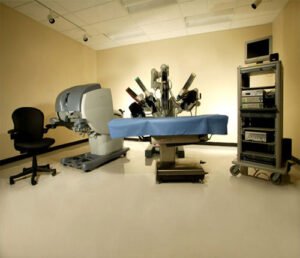
Robot-Assisted Radical Prostatectomy
For those who can afford it, robotic surgery is the most advanced method to remove the prostate. However, the surgeon’s expertise is more important than the robotic system itself. While open surgery is also effective, it typically requires a longer hospital stay and has slightly higher blood loss compared to robotic surgery.
Possible Complications After Surgery
- Sexual Impotence: Depending on the stage of cancer, there is a risk of losing the ability to achieve an erection. In cases of localized prostate cancer, 60% of men regain potency within a year. However, even if potency is regained, ejaculation will not occur (a condition called dry orgasm).
- Urinary Incontinence: The prostate sits on a valve (sphincter) that controls urine flow. Removing the prostate can weaken this valve, leading to urine leakage. About 90% of patients regain control within three months, but 1-3% may experience persistent leakage beyond one year. Surgical options are available for those with persistent incontinence.
Role of Endoscopic or Laser Surgery
Endoscopic or laser surgery is primarily used for benign prostatic hyperplasia (BPH). However, in cases of metastatic prostate cancer with urinary obstruction, these procedures may be performed to create a passage for urine flow.
Best Treatment for Metastatic Prostate Cancer (Group 3)
The standard treatment for metastatic prostate cancer is Androgen Deprivation Therapy (ADT), which reduces testosterone production, the primary fuel for prostate cancer growth. More than 95% of patients respond well initially, with PSA levels returning to near normal. However, over time, cancer cells find alternative growth mechanisms, leading to Castration-Resistant Prostate Cancer (CRPC).
Treatment for Castration-Resistant Prostate Cancer (CRPC)
For CRPC, newer drugs can improve survival and quality of life. Options include:
- Abiraterone
- Docetaxel
- Enzalutamide
- Denosumab
- Immunotherapy
These drugs may be used alone or in combination, based on the patient’s condition and treatment goals.
Final Thoughts
Prostate cancer, if detected early, is highly treatable. Regular screening, maintaining a healthy lifestyle, and consulting a urologist for appropriate tests can help in early detection and better outcomes. If diagnosed, discussing all treatment options with a specialist is essential for making an informed decision.
